Abstract
Introduction: In multiple myeloma (MM) the bone marrow (BM) microenvironment, plays an important role in mediating survival, proliferation, resistance to therapy as well as disease evolution. The BM microenvironment is mainly composed of mesenchymal stromal cells (BM-MSC), endothelial cells, immune cells, and extracellular matrix. BM-MSC can acquire distinct functional phenotypes that are influenced by signals in the microenvironment and have been shown to facilitate MM development and drug resistance through cell-cell contact and cytokine secretion. However, little is known about the mechanisms of immune modulation mediated by BM-MSC in the inflammatory MM tumour microenvironment (TME). Aberrant glycosylation is a hallmark of cancer cells, playing an important role in tumor progression. Our data strongly links aberrant sialylation with poor prognosis in MM (1) but to date the immunological consequences of this phenomenon have not been explored. Here we sought to investigate if regulation of BM-MSC sialylation alters their ability to inhibit effector T-cell function in an inflammatory microenvironment, characteristic of the MM TME.
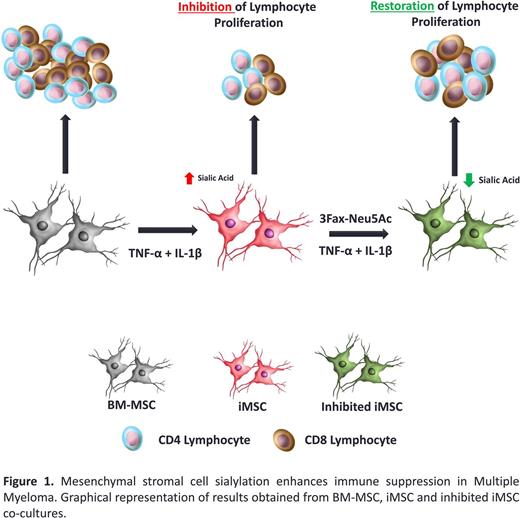
Methods: BM-MSC were isolated from BALB/c mice and extensively characterized in vitro . Since inflammatory mediators, such as TNF-α and IL-1β are present at high levels in MM due to constitutive NF-kappaB activity, we assessed the effects of both of these pro-inflammatory mediators on BM-MSC phenotype. BM-MSC were treated with both tumor necrosis factor alpha (TNF-α 50ng/ml) and interleukin 1 beta (IL-1β 50ng/ml) (iMSC) for 72 hours and cell surface sialylation was analysed by flow cytometry. To determine immunoregulatory ability, BM-MSC and iMSC were co-cultured in mixed lymphocyte reactions (MLRs) for 96 hours. T-cell proliferation, activation, death and differentiation were determined by flow cytometry. To determine the role of increased sialylation in lymphocyte suppression, both BM-MSC and iMSC were pre-treated with a sialyltransferase inhibitor (3Fax-Neu5Ac) for 72 hours prior to TNF-α and IL-1β stimulation. To determine the important of antigen presenting cells in sialic acid dependent regulation of T cell phenotype, CD11c+ and CD11b+ innate immune cells were removed via MACS sorting prior to co-culture. BM-MSC: Lymphocyte co-culture supernatants for nitric oxide (NO), IL-10 and PGE-2 were analysed by ELISA.
Results: iMSC displayed significant phenotypical changes with CD73 and CD44 increasing significantly. Both SCA-1 and CD105 were significantly reduced. No changes in cell viability were noted after pre-treatment and no significant changes in proliferation were observed. iMSC had significantly increased levels of both α2-3 and α2-6 linked sialic acid when compared to BM-MSC. In vitro, iMSC displayed an enhanced ability to inhibit lymphocyte proliferation when compared to BM-MSC alone. iMSC significantly inhibited the proliferation of hyper-stimulated CD3+CD4+ and CD3+CD8+ lymphocytes. 3Fax-Neu5Ac treated BM-MSC and iMSC displayed no significant changes in phenotype, viability, proliferation and cell size. However, following sialyltransferase inhibition, iMSC lost the ability to suppress both CD3+CD4+ and CD3+CD8+ lymphocytes resulting in significant restoration of lymphocyte proliferation. This restoration of proliferation was further enhanced in the absence of CD11c+ and CD11b+ innate immune cells. Cell surface sialic acid expression correlated with both CD3+CD4+ and CD3+CD8+ lymphocyte suppression. No changes in soluble mediators of BM-MSC immunomodulation, such as nitic oxide, IL-10 and PGE-2 were observed suggesting that restoration in proliferation was both sialic acid and cell-contact dependent.
Conclusions: Our findings confirm inflammation, characteristic of the MM TME, induces BM-MSC sialylation and enhances their ability to suppress activated adaptive and innate immune effectors. Understanding the potential utility of targeting BM-MSC sialylation and consequently their immunomodulatory potential, may enhance immune cell activation in the MM microenvironment, providing further rationale to targeting BM-MSC sialylation in the context of MM. We suggest that understanding the functional importance of the BM stroma and its interaction with MM and immune cells is likely to lead to the identification of sialylation, as a new molecular target.
Glavey SV, et al Blood. 2014 Sep 11;124(11):1765-76
Ryan: Janssen: Research Funding. O'Dwyer: Onkimmune Ltd: Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; GlycoMimetics Inc: Research Funding; Janssen: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal